Minimizing Risks
In everything we do in life, there are certain risks involved. Some things are of higher risk than others. Our job is to minimize these risks in our lives.
When crossing the street, we stop and look both ways. If we see that no car is coming and the crossing is safe, we continue on across the street. Here we are minimizing our risks involved in crossing the street instead of blindly jumping out in the busy road without looking.
This pertains to eye care also. Many people are in higher risk groups than others for a variety of reasons whether it be by choice, as in contact lens wear or due to a genetic predisposition to a particular ocular disease. Our job as responsible people is to properly minimize the risks involved in our eye health in any way possible to assure ourselves that our eyes will last and serve us well. Not all conditions can be detected without an examination, until it is too late. Prevention is the key to good health risk management.
The Internet is an easy place to find health-related information, but how can you know that what you’re finding is credible? As a rule, health-related sites sponsored by the U.S. government (Web addresses ending with “.gov”), not-for-profit health or medical organizations (ending with“.org”) and university medical centers are among many reliable sources of health information on the Web. You can also look for the red and blue “HON” seal, which means that a site meets certain standards set by the Health On the Net Foundation.
Kids At Risk
Children born prematurely or with low birth weights are at higher risks and should be evaluated at 6 months of age or sooner. Those with parents who have significant visual correction should be monitored early and regularly. Kids who are physically or mentally challenged are also in a higher visual risk group.
Contact Lens Wearers
Contact lens wear by itself is a very safe practice if done responsibly. As a contact lens wearer, you are exposed to a risk of eye infections and trauma. To minimize these risks, have your eyes checked regularly. Our doctors stress that you must also follow directions for wearing time, solution use and replacement of lenses. Wearing lenses longer than they are designed, significantly increases the risk of sight-threatening ocular infections.
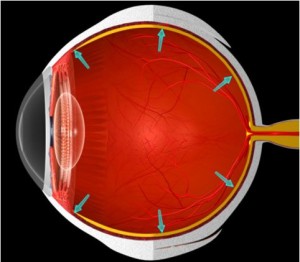
Highly nearsighted patients
Oftentimes nearsightedness is caused by a larger eyeball. This extra length of the eye may cause the retina (the seeing part) to be stretched, pulled and thinned. This stretching can put you in a higher risk group for retinal detachment which may cause blindness. To minimize the risk of this occurring, must have regular checkups to have your eyes examined for the health of the retina. If discovered early enough, loss of vision may be prevented.
Glaucoma & Glaucoma suspect patients
Glaucoma is often called the “silent thief” since it slowly steals your vision without you even realizing it, until it is far too late. You can minimize your risks by having appropriately timed and proper tests to detect any changes which could lead to vision loss. If detected early loss of vision can be prevented by a variety of means.
Diabetic patients
Diabetes is the leading cause of blindness. Most often from the “leaking” of blood vessels in the eye, which depletes the tissue of necessary oxygen and nutrients. With this depletion comes the death of the tissue and ultimately loss of sight. It is critical that diabetics be monitored regularly, we can discover any leaking blood vessels and have them sealed through the use of a laser, thus allowing the normal flow of blood to the tissue.
Cataract patients
Cataract patients must have regular checkups to evaluate the growth of the cataract and to evaluate the overall health of the back of the eye before the cataract becomes so dense that the back of the eye can not be seen. Cataracts are well managed today and can be a opportunity for many patients to reduce their dependency on glasses and contacts.
Here are some common eye aliments and things to consider.
Click on a topic for more information
Allergies
If your eyes are red, swollen, or itchy, either seasonally or after exposure to certain things, it is likely that you have some allergies that affect your eyes.
Rinse your eyes with over-the-counter eye washing solutions such as Blinx, Collyrium, or Tears Naturale. What you accomplish is ridding the eye of the allergen-dust, mold, cat hair, or whatever is bothering you.
 Avoid using Visine or Murine or any solution that “gets the red out,” because they give only temporary relief from redness without solving your problem. Dr. Baron and many other eye doctors do not recommend them.
Avoid using Visine or Murine or any solution that “gets the red out,” because they give only temporary relief from redness without solving your problem. Dr. Baron and many other eye doctors do not recommend them.
Put cold packs on your eyes to reduce swelling and itching.
Use refrigerated NON-preserved artificial tears hourly to sooth and flush the eyes.
Consider trying over-the-counter antihistamines such as Chlor-Trimeton or Benadryl. If you find this beneficial, you may want to consult your general physician to prescribe other antihistamines.
If you can determine what you are allergic to, such as cat hair, ragweed, pine pollen, dust, or mold- try to avoid contact with any of them to minimize the problem.
Consider using glacier type glasses with side shields when outdoors during high pollen seasons.
Blepharitis
 The medical term blepharitis refers to inflammation in a person’s eyelids. Although usually not sight-threatening, it can cause significant discomfort and subtle infection. Blepharitis is a chronic (no cure) disease, but daily treatment can minimize it.
The medical term blepharitis refers to inflammation in a person’s eyelids. Although usually not sight-threatening, it can cause significant discomfort and subtle infection. Blepharitis is a chronic (no cure) disease, but daily treatment can minimize it.
The site of the inflammation in the lid are tiny glands on both the upper and lower eyelids. These glands produce a clear oil that is part of the tear film of the eye. When a person has blepharitis, this oil changes to a thick greasy consistency which can then plug the oil glands causing styes and other minor problems. Even if it does not plug the gland, the greasy secretions accumulate on the lashes and traps debris, bacteria and produces side effects.
Fortunately, the treatment is relatively simple and can be built into your schedule without inconvenience. The answer is good lid hygiene.
To avoid blepharitis patients should use hot, moist lid scrubs. This involves placing a clean washcloth under warm tap water, add a dab of baby shampoo and gently rubbing the closed lids where the eyelashes exit.
Our doctors suggest this should be done at least once each day. Although antibiotics may be of some help during the early treatment of blepharitis, they are much less important than effective and continued lid hygiene.
Your adherence to this procedure will give you healthy comfortable eyes, free of complications from blepharitis.
Cataracts
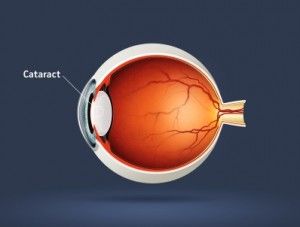 A cataract is any loss of clarity in the lens of the eye, like looking through a dirty window. Furthermore, it can cause colors to shift or appear very dull and difficulty in seeing slopes and stairs. The degree that it affects a person varies from minor to severe.
A cataract is any loss of clarity in the lens of the eye, like looking through a dirty window. Furthermore, it can cause colors to shift or appear very dull and difficulty in seeing slopes and stairs. The degree that it affects a person varies from minor to severe.
The benefit of more birthdays is normally the most common cause of cataracts, if we live long enough we will all get cataracts. They are influenced by nutrition, certain medicines, ultraviolet (UV) light, heritage, trauma to the eye, and illnesses.
During the early stages of cataract development patients might notice a glare, a haze, or a general cloudiness of vision. Cataracts do not cause pain or discomfort. They are not cancerous or tumorous. They are not an emergency.
Changes in your eye sight may be so small and subtle that you may be only slightly aware of them. Many times there will be a shift in your prescription and it will appear that you are becoming more nearsighted. This phenomenon is the RULE rather than the exception and is often called “second sight”.
 Regular primary care eye examinations are recommended to keep your vision as sharp as possible. We provide independent unbiased advice regarding surgery.
Regular primary care eye examinations are recommended to keep your vision as sharp as possible. We provide independent unbiased advice regarding surgery.
If your sight becomes bad enough or if you are having noticeable problems with vision interfering with your life style, then we may advise you to have cataract surgery. Generally, cataract surgery is an outpatient procedure with only a few restrictions on activities following surgery. Insurance may take care of most of the cost and you should check to get the exact amount covered from the surgeon. A full explanation of the pros and cons will be given to you along with the potential increase in vision expected with the surgery from the surgeon. We have observed the results of many surgeons and their techniques we are in a position to recommend the best surgeons in the Rocky Mountain Region.
Cataract surgery is the most common surgical procedure in the United States and has a very high success rate. The result of the surgery can improve your vision considerably.
 During the cataract surgery an implant (artificial plastic lens) is placed into the eye. This is desirable because prior to the use of implants, patients needed to have very thick glasses or use contact lenses. Neither arrangement was extremely efficient or natural. Following cataract surgery, glasses are still needed, but their appearance and use is similar to what you experienced prior to surgery. The final benefit from the surgery cannot be fully appreciated until the glasses are prescribed, and it is usually recommended that you wait 3-4 weeks, as fluctuations in vision happen due to the healing process. In high percentages (80-85%) the prescription will change again in about a year. For this reason our doctors suggests yearly re-evaluations.
During the cataract surgery an implant (artificial plastic lens) is placed into the eye. This is desirable because prior to the use of implants, patients needed to have very thick glasses or use contact lenses. Neither arrangement was extremely efficient or natural. Following cataract surgery, glasses are still needed, but their appearance and use is similar to what you experienced prior to surgery. The final benefit from the surgery cannot be fully appreciated until the glasses are prescribed, and it is usually recommended that you wait 3-4 weeks, as fluctuations in vision happen due to the healing process. In high percentages (80-85%) the prescription will change again in about a year. For this reason our doctors suggests yearly re-evaluations.
30% may develop a secondary cataract, which can be remedied by quick and easy. This minor complications is removed with a laser surgery. Initial cataracts cannot be removed by lasers.
If you have special concerns, problems, or questions please call our office. We want you to understand this condition and the procedures that can be done to improve your sight. Your vision is our primary interest.
See how sunglasses can help reduce your risk of getting cataracts.
Contact Overuse Syndrome
Abusing wear contact lenses can permanently affect your sight or ability to wear contact lenses for the remainder of your life.
The short term effects of over wearing your extended wear contact lenses are red, painful eyes and occasionally poor vision. If this ever happens to you, immediately remove your lenses and call our office. If these symptoms are ignored or simply waived off as “temporary” or “It’ll be gone by the morning”, you move into a higher risk zone with a potentially permanent loss of vision. New blood vessels may grow into the cornea which can mean permanent loss or the ability to wear contact lenses. The worse case scenario would be the development of a corneal abrasion which becomes infected and ulcerates, causing a permanent scar. If this occurs in the center of your cornea where you look through, it may cause such a vision loss that the eye is legally blind.
As you can see, playing the extended wear game by your rules and not the recommendations of the FDA, AOA, and AMA is dangerous. There are no guarantees that noncompliance will lead to this severity, but you are certainly putting yourself into a high risk category with which we are not comfortable.
Recommendations:
- Wear extended wear contacts only 6 days maximum.
- Leave your lenses out 18 hours + per week, so they can obtain enough Oxygen with your eyes open.
- Replace contact lenses as prescribed.
- Be evaluated every 3 months, as long as you wear the lenses overnight.
- Put drops in your eyes at bed time and upon arising, andcleans lens well.
You can learn more about contact lenses on our contact lens page or by contacting the office at 303-728-20/20
Diabetes and Eyes
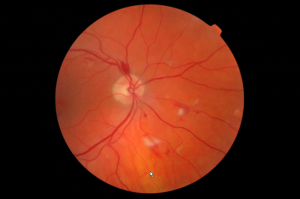 If you have a diabetic condition or know someone who does, you are probably aware of the fact that diabetes can interfere with the body’s ability to break down sugar.
If you have a diabetic condition or know someone who does, you are probably aware of the fact that diabetes can interfere with the body’s ability to break down sugar.
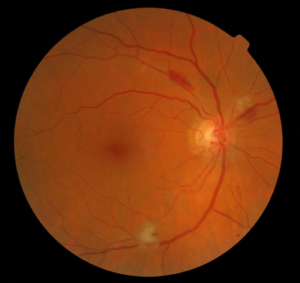
Over time, this condition can weaken the lining of small blood vessels in the body and cause them to change and leak. When this occurs in the retina of the eye, it is called diabetic retinopathy. Early diagnosis and treatment is essential, since this eye disease can lead to blindness. That’s one reason why it is important to have your eyes examined annually by a doctor of optometry if you are a diabetic.
A thorough, comprehensive eye examination consists of several tests and procedures. During this time we are getting to know you, be sure to mention your family history of diabetes so we can rule out any signs of the disease. Not every diabetic patient develops retinopathy, but the chances of getting it do increase after having diabetes for several years. Evidence also suggests that factors such as pregnancy, high blood pressure and smoking may cause diabetic eye disease to develop or worsen. Diabetic retinopathy describes all the types of blood vessel changes that can occur inside the retina due to high blood sugar levels. The duration of elevated blood sugar levels can also cause these changes. This condition usually affects both eyes at the same time and develops in stages.
The beginning stage may produce visual symptoms like blurriness in your central and peripheral (side) vision, or it may produce no visual symptoms at all. It mainly depends on where the blood vessel changes take place inside your eye’s retina, which is a light-sensitive tissue lining the back of your eye that sends visual messages to the brain. As diabetic retinopathy progresses, you may notice a cloudiness in your vision, floaters or blind spots. This is usually caused by blood, leaking from abnormal new blood vessels, which blocks light from reaching the retina. In the advanced stage, connective scar tissue forms in association with new blood vessel growth, causing additional vision distortion and blurriness. With time, this tissue can shrink and detach the retina by pulling it towards the center of the eye and away form its underlying structure.
Once diabetic retinopathy has been diagnosed by our doctors or your family physician, laser and other surgical treatment may be used to reduce the progression of this eye disease and decrease the risk of vision loss. Ask us to explain the types of treatment available and those best suited to your situation. If diabetic retinopathy should impair your ability to see, we may prescribe special low vision aids to help maximize your remaining vision. Some of the optical aids available include telescopic lenses for distance vision, microscopic lenses, magnifying glasses and electronic magnifiers for close work. All are available here at Golden Vision Clinic.
As a diabetic, or person at risk, it is important that you take steps to help prevent the development of diabetic retinopathy and to help maintain a healthy body. One of those is having periodic eye examinations. Others include taking prescribed medication correctly, following a proper diet, and exercising regularly. By following these guidelines, chances are good that you can enjoy a lifetime of good vision and health.
Dry Eyes
 Dryness is the result of the eyes being inadequately lubricated by tears. Dryness can cause red eyes. These conditions of the eyes usually are chronic, long term, mild to moderate irritations that after 5-10-20 years, leave your eyes in poor health and poor appearance. Redness of the eye occurs when the exterior blood vessels in the eye become dilated due to overexposure to sun, wind, dust, allergies, irritants or infections. Our doctors recommend that you take this situation seriously NOW and do all you can daily to minimize the effects of this with time. Other factors causing either, or both, of these conditions are:
Dryness is the result of the eyes being inadequately lubricated by tears. Dryness can cause red eyes. These conditions of the eyes usually are chronic, long term, mild to moderate irritations that after 5-10-20 years, leave your eyes in poor health and poor appearance. Redness of the eye occurs when the exterior blood vessels in the eye become dilated due to overexposure to sun, wind, dust, allergies, irritants or infections. Our doctors recommend that you take this situation seriously NOW and do all you can daily to minimize the effects of this with time. Other factors causing either, or both, of these conditions are:
1. LOW TEAR VOLUME: Tears are the eyes’ natural lubricant, keeping them moist and clear. A low tear volume and quality may cause eyes to become dry and uncomfortable. Tears are composed of a layer of mucin (which holds the tears to the eye), water and nutrients (composing the major part of the tears), and oil (the top layer, which keeps the tears from evaporating). If this composition is out of proportion, your eyes may feel discomfort. Maintaining your health, through diet and vitamins, can help maintain these tear layers. The volume of tears can be improved through normal consumption of water. A common symptom of dry eyes is occasional excessive tearing! This is an attempt by your eyes to compensate for the dryness. We recommend drinking two glasses of water before each meal or more (10 8oz glasses/day), to help increase the volume of your tears, and also decreasing your salt consumption. People who drink coffee, tea, sodas (especially diet sodas), or alcohol (which are all diuretics) pass more fluid than they drink. Normally one should drink 32+ ounces of water per day, if you exercise, you should also increase your consumption accordingly.
2. VITAMIN A: It is best that you take a Multi-Vitamin as your base supplement, then add what you need from that point, as all the vitamins are inter-related in their functions and utilization. Vitamin A is a very important vitamin for the eyes; however, it can become toxic at high dosages. We suggest that you try up to 10,000 units per day, for 4‑6 weeks, and then we will evaluate how you are doing. For dosages above 10,000 I.U., a physician should be consulted first. Beta Carotene is the precursor to Vitamin A and can be taken in capsule form or is found in vegetables and fruits; your body converts it to Vitamin A as needed. Recommended daily intakes of Beta Carotene are 5 to 10 mg. If you are a smoker or are around smokers DO NOT take Beta Carotene, as it has been linked to causing lung cancer. It would be wise to take Vitamin A or Beta Carotene in combination with a multi-vitamin so your body will utilize all the factors for the best and ideal effect. . . and remember all those bright yellow & orange fruits and green leafy vegetables!
 3. ARTIFICIAL TEARS: Artificial tears are used to supplement the tears and to help moisten the eyes; however, they do not take the redness out of the eyes. Reasons for using artificial tears are dryness of the eyes due to environment, a closed room with forced‑air ventilation, medication, hormonal changes, allergies, and pinguecula. Three suggestions for this type of product are ReFresh, Systane, or Optive. Use as often as needed; 3-4 times a day is common. Those products that claim to “take the red out” are not recommended, because of a reaction they induce called the “rebound effect.” The drug used is a vasoconstrictor, which decreases the size of the blood vessels temporarily. However, when the drug wears off, the blood vessels will dilate to a greater size than they were originally, leading to constant use of “whitening” drops. However, if used rarely, these products will not harm your eyes.
3. ARTIFICIAL TEARS: Artificial tears are used to supplement the tears and to help moisten the eyes; however, they do not take the redness out of the eyes. Reasons for using artificial tears are dryness of the eyes due to environment, a closed room with forced‑air ventilation, medication, hormonal changes, allergies, and pinguecula. Three suggestions for this type of product are ReFresh, Systane, or Optive. Use as often as needed; 3-4 times a day is common. Those products that claim to “take the red out” are not recommended, because of a reaction they induce called the “rebound effect.” The drug used is a vasoconstrictor, which decreases the size of the blood vessels temporarily. However, when the drug wears off, the blood vessels will dilate to a greater size than they were originally, leading to constant use of “whitening” drops. However, if used rarely, these products will not harm your eyes.
4. LID MASSAGE: Some people have stagnation of the glands underneath the eyelids. When this occurs, the tear quality changes by becoming too full of mucus, causing the eyes to dry out faster. One remedy that has been found to be successful is lid massage. This can be done while washing your face, by placing a hot washcloth on your eyes and massaging the upper lid against the upper bone and the lower lid against the lower bone, around your eye. This need not take more than five or ten seconds daily and, with time, the massage and the heat will open the glands, bringing the tear quality and quantity back to its normal level.
5. BLINKING: Blinking is the windshield wiper of your eye and one of its purposes is to evenly and regularly spread tears over your eyes to keep them wet, seeing clearly, and healthy. Computer operators have been found to blink only 3 times per minute rather than the normal 15 times per minute. Contact lens wearers also can adopt an abnormal blink rate and pattern. Please be aware of this and enhance your blink pattern, rate, and read about blinking on our contact lens page.
6. MEDICATIONS: Various medications can dry mucous membranes, including those in the eyes, causing red and dry eyes. Please inform us of any medications that you are now taking, any you have recently stopped taking or any that you have changed (i.e. antihistamines and diuretics).
7. SMOKING: Whether you or those around you indulge in smoking, it is important that you minimize (if not eliminate) your exposure. Smoking is a definite an irritant to the eyes. Also be aware, Beta Carotene has been linked to causing lung cancer in smokers and others exposed to second hand smoke.
8. EXPOSURE TO THE ELEMENTS: Exposure to the sun and wind is very hard on the eyes. The use of high quality, properly tinted sunglasses eliminates the harmful ultraviolet and infrared wavelengths caused by overexposure. This is especially true for those of us who work and play outdoors at these high altitudes in Colorado. Overexposure is believed to accelerate the development of cataracts and break down of the retina. Check out ways to limit your eyes’ exposure in our optical boutique.
9. HEAT/AIR CONDITIONING: Office and other indoor environments have controlled air vents for heat and air conditioning, which rapidly dry the eyes. If possible, face away from the duct or vent to eliminate that direct exposure. Use a personal humidifier and artificial tears as necessary.
10. FLUORESCENT LIGHTING: Most offices and business use fluorescent lights. Many people find this type of lighting bothersome and irritating to the eyes. We recommend a pink tint in your glasses, or tinted contact lenses, to reduce the glare and balance the wavelengths. There are also new generations of Anti-Glare coatings that reduce the affects of fluorescent lights.
11. FULL SPECTRUM LIGHT: There is a theory emerging that espouses the need of a full spectrum of light every day. Regular fluorescent lights are not full‑spectrum; there is a light called Vita-lite and Ott-lite that meets this criterion. The use of this type of light may be beneficial for people with red eyes.
12. CONTACT LENS WEAR: If you are a firm contact lens wearer, you may need to have old or scratched contact lenses polished or replaced, because they will not wet properly, causing eye discomfort. If you are a soft contact lens wearer, using some of the older solutions, it might be wise to consider updating to the newer solutions. The best soft lens solutions are Clear Care to disinfect your lenses and “aerosol saline” to rinse, both of which eliminate the potential of allergic reactions to preservatives, which can cause red eyes.
13. CURRENT PRESCRIPTION: Make sure you have an up-to-date prescription in glasses, so you are not straining your eyes while wearing them.
14. VISION THERAPY: If your eyes have poor visual skills, are working inefficiently as a team, have focusing problems, or are strained by doing extensive visual tasks, it may be wise to increase these abilities through vision therapy. Efficient functioning of the eyes should facilitate the decrease of red eyes caused from eye strain.
15. OCULAR OINTMENT: If tears and supplemental tears are not enough to relieve dry eye problems, a sterile ophthalmic ointment can be used. Unless otherwise instructed, use at bedtime, for your vision will be very blurry. Wash your hands, then put a small amount on your index finger, place the ointment on the lower inside lid of both eyes. In the morning, use a warm washcloth to clean your lids and lashes.
16. NEW DIAGNOSTIC TEST: In the event that your eyes are still dry after all the alternatives are pursued as prescribed, a new diagnostic test is available. The drainage system in one eye is temporarily plugged with a collagen plug which slowly dissolves so that we can determine if the flow of the tear gland is sufficient with the drainage system closed. The test usually runs over a two‑week period. If this closing of the drainage system proves helpful, semi‑permanent closure can be accomplished through non-dissolvable plugs. We use the collagen plugs to test whether such closure is of slight or significant value.
17.NEW MEDICATIONS: There now is a prescription medication, Restasis, that is FDA approved to increase the quality and quantity of you natural tears. This medication is a commitment. It can take up to 3 months to notice the benefits of the treatment. It also is only available as the name brand medication (no generic) and can be expensive, although their are cost savings programs through the drug manufacturer.
We are happy to answer any additional questions at an examination or through phone or email.
Flashes and Floaters
 Spots and floaters are very common. Almost everyone sees a few spots at one time or another. The inner part of the eye is made up of a clear, jelly-like fluid known as the vitreous. As time goes by the vitreous begins to shrink and liquify causing us to see floaters. These floaters are easily seen when looking at a lighter background such as the sky or a light colored wall. If you try to look at the spots directly, you will never be able to actually “catch up with them.” They may be of various shapes and sizes and appear as thread like strands or cobwebs within the eye. Most floaters are normal and rarely themselves cause blindness.
Spots and floaters are very common. Almost everyone sees a few spots at one time or another. The inner part of the eye is made up of a clear, jelly-like fluid known as the vitreous. As time goes by the vitreous begins to shrink and liquify causing us to see floaters. These floaters are easily seen when looking at a lighter background such as the sky or a light colored wall. If you try to look at the spots directly, you will never be able to actually “catch up with them.” They may be of various shapes and sizes and appear as thread like strands or cobwebs within the eye. Most floaters are normal and rarely themselves cause blindness.
But, some spots may be caused by certain serious injuries or eye disease. Thus patients seeing floaters not seen before, a sudden increase in the size or number of floaters or flashes of light with or without the floaters, should have a vision examination to determine the cause immediately. To make sure these are not retinal detachments, the doctor will look into your eye extensively with lighted instruments to observe the spots. If there is a concern for your eyes health or vision, the appropriate care will be recommended.
There is no treatment for spots and floaters if the cause is from shrinking and liquefaction of the vitreous. This is simply a change we see with birthdays. Sudden changes in the appearance of floaters and flashers may indicate a retinal tear or more significant problem.
 SYMPTOMS OF RETINAL TEARS TO WATCH FOR:
SYMPTOMS OF RETINAL TEARS TO WATCH FOR:
FLOATERS: Sudden strings, spider webs, or dots in the vision. Patients who already have some floaters in their vision should watch for sudden, dramatic increase in these.
FLASHES OF LIGHT: Bright flashes of light resembling lightning, which often appear off to the side of the vision.
DIMMING OF THE SIDE VISION: A dim or gray area developing in the side vision in any direction, resembling a curtain being drawn.
If you experience any of these symptoms, please contact the office immediately at 303-278-20/20
Glaucoma
Being a glaucoma suspect does not mean you have or ever will have glaucoma. It does mean, however, that because of some of the results of your tests or family history, you have a higher potential or some risk factors of developing glaucoma.
 Glaucoma is basically a plumbing problem in the eye, and rarely presents any symptoms. It is caused by the unrelieved pressure of fluid in the eye. There is a structure in the eye that produces fluids and helps to nourish and keep it firm. This fluid must drain out of the eye, in order to maintain a healthy eye pressure. Some people have a large drainage angle from which this fluid must drain, while others have a medium or small angle. If untreated it slowly destroys the side vision, and, by the time the patient is aware of it, it is irreversible.
Glaucoma is basically a plumbing problem in the eye, and rarely presents any symptoms. It is caused by the unrelieved pressure of fluid in the eye. There is a structure in the eye that produces fluids and helps to nourish and keep it firm. This fluid must drain out of the eye, in order to maintain a healthy eye pressure. Some people have a large drainage angle from which this fluid must drain, while others have a medium or small angle. If untreated it slowly destroys the side vision, and, by the time the patient is aware of it, it is irreversible.
Although glaucoma cannot be cured, it can be controlled by eye drops, which may be used to decrease the fluid production, or to help open the drain. Rarely is surgery necessary.
We recommend that if you are a glaucoma suspect, you should be evaluated more frequently than usual. It is highly advisable that you have a glaucoma workup every 3, 6 or 12 months, depending upon your risk factors. If monitored and cared for there should be no concern of visual loss. Anyone can diagnose glaucoma when it is too late and you have lost half of your vision. Today we have the knowledge, techniques, and sophistication to monitor even slight changes of visual loss, to enable us to start care before any significant loss occurs.
If you are a narrow‑angle glaucoma suspect, you should be aware of (and act on) the following:
1. Advise your physician and dentist so that they are very careful not to prescribe drugs that might precipitate an attack of glaucoma.
2. If you have an extremely painful eye, go to an emergency room and tell them you may be having an acute glaucoma attack. Fortunately, this is a rarity. The damage to your eye is related to time; by having the high pressure reduced quickly, you should have no, or minimal, damage to your eye.
3. Conversely to #2, you may be unaware of slightly elevated pressure for years and, unfortunately, this can cause serious visual loss. This is a reason for frequent check‑ups.
4. If you have a dull aching eye, upon awakening, call our office first thing in the morning for a pressure check as soon as possible. Eye pressure is often highest early morning.
Have periodic recommended workups, to prevent loss of vision. In this situation, it is better to be safe than sorry!
In our office we will evaluate you for glaucoma in several ways:
TEST FOR PERIPHERAL VISION: This is done, routinely, to check your peripheral field of vision. If loss occurs, it happens so slowly that one is rarely aware of any vision loss.
INTERNAL EYE EVALUATION: This is also done, routinely, with a special instrument called an ophthalmoscope, which evaluates the structure of the interior of your eyes. In glaucoma, the internal eye pressure increases and pushes on the optic nerve head. This area is carefully studied with this instrument, to make sure all is as it should be.
ANGLE OF OUTFLOW: In order to keep your internal ocular pressure within normal limits, the angle of outflow (like a sink drain or a safety valve) must be open and clear. Details of this area are studied with a powerful microscope.
TONOMETRY: This test is performed on all patients over thirteen years of age, routinely, and others, when indicated. We use a non‑contact tonometer, which is quick and painless. It measures the actual pressure within your eye and gives us a digital readout, which is then compared with normal pressure ranges.
Further evaluation may also include
GOLDMAN TONOMETER: If the pressure within your eye is high or questionably high, we use the Goldman tonometer to re‑check it. This very quick and accurate method for measuring pressure is used with a powerful microscope and special dye. The reading will also be compared with normal pressure ranges.
VISUAL FIELDS STUDY FOR GLAUCOMA: Our computerized, peripheral visual field instrument has a specific program which evaluates the areas that are damaged by high eye pressure from glaucoma. This instrument painlessly maps out your peripheral field of vision, in order to measure its quantitative and qualitative extent. It can reveal even very small amounts of damage resulting from glaucoma.
FUNDUS PHOTOGRAPHY: A picture of the internal eye is taken and kept on file for future comparisons.
PACHYMETRY: This instrument measures the corneal thickness to accurately calibrate you eye pressure reading.
DIURNAL VARIATIONS: The pressure in your eye varies throughout one day, hopefully within the normal ranges. If the pressure changes greatly throughout one day, your eye may not be able to withstand this continual increase and decrease of pressure. We are able to determine these variations by measuring your pressure three times in one day (9:00 a.m., noon, and 5:00 p.m.).
OPTICAL COHERENCE TOMOGRAPHY: This state of the art instrument takes very detailed measurements of the nerves in the back of your eye. We can use it to watch for changes in the optic nerve and the nerve fiber that carry the signal from the retina.
Learn more about the specific procedures and our instruments on our vision tools page.
High Blood Pressure & Eyes
Your retina is the only place in your body that live blood vessels can be viewed without actually cutting any tissue. When we examine your eyes, we check for the signs that indicate whether your blood pressure has been high for an extended period of time. Often, people with uncontrolled high blood pressure experience changes in the back of both eyes and may never notice any difference in their vision.The long term effects of chronic high blood pressure on the vasculature that nourishes your eyes may take 10-30 years to develop. Maintaining a good blood pressure is the best way to keep your vessels healthy.
 An analogy can be made comparing your blood vessels to a rubber hose. If a rubber hose is rated for 90 pounds/square inch and the actual pressure is greater, the hose may burst. Whatever device the hose is supplying will no longer be functional. If an artery supplying your heart bursts, it is called a heart attack. A stroke is caused by a burst blood vessel in the brain, and if a blood vessel that supplies the eye bursts, it may lead to partial or complete blindness to that eye.
An analogy can be made comparing your blood vessels to a rubber hose. If a rubber hose is rated for 90 pounds/square inch and the actual pressure is greater, the hose may burst. Whatever device the hose is supplying will no longer be functional. If an artery supplying your heart bursts, it is called a heart attack. A stroke is caused by a burst blood vessel in the brain, and if a blood vessel that supplies the eye bursts, it may lead to partial or complete blindness to that eye.
There are many ways that high blood pressure can be controlled, depending on the severity. It may only take a mild exercise program combined with nutritional changes that include reduced salt and fat intake. Lifestyle changes may be recommended to help reduce stress. These must be done slowly and one at a time. Advanced medical therapy is also available for conditions that are unresponsive to non-medicinal methods. Routine health care is recommended so that professionals can monitor your progress and make further recommendations. It is important that you have a complete physical examination on a regular basis with your primary care physician. If you have not had one recently, you should arrange to have one at your medical doctor’s office.
If you need a referral, we can arrange this with one of many excellent local physicians.
Injuries
 Our eyes are protected by the bony structures that create the eye socket; within this socket we have protective fatty tissue, and our lids and lashes protect the front eye surface. Despite these protective structures, there are many sports, industrial, and home eye injuries each year.
Our eyes are protected by the bony structures that create the eye socket; within this socket we have protective fatty tissue, and our lids and lashes protect the front eye surface. Despite these protective structures, there are many sports, industrial, and home eye injuries each year.
In sports, especially racquet and fast-moving ball sports, it is imperative to wear proper protective eyewear. In industry, safety eyewear is required by OSHA in any eye hazard situation. At home, safety glasses should be worn by anyone operating shop machinery equipment, working with cleaning agents, mixing any chemicals or working below falling or potential dropping objects (car repair, tree trimming, weeding and sun protection). Wear sun safety glasses while gardening.
An eye or head injury can affect any eye structure. It is very important for immediate proper care after an injury.
 External injuries are easy to see: a bump or bruise; internal injuries are not as easy to detect but can be associated with some visual symptoms, flashes of light , increase in floating spots or a curtain covering your vision, to name a few. If any of these symptoms occur, you need to be seen immediately. All injuries to your eyes need to be evaluated to insure no immediate damage. However, please keep in mind that follow up care is just as important because the highest incidence of retinal detachment due to trauma occurs up to 18 months after the initial injury.
External injuries are easy to see: a bump or bruise; internal injuries are not as easy to detect but can be associated with some visual symptoms, flashes of light , increase in floating spots or a curtain covering your vision, to name a few. If any of these symptoms occur, you need to be seen immediately. All injuries to your eyes need to be evaluated to insure no immediate damage. However, please keep in mind that follow up care is just as important because the highest incidence of retinal detachment due to trauma occurs up to 18 months after the initial injury.
The best choice is to prevent eye injury with protective eye wear. The best insurance after an injury is a through examination and proper follow up care.
Reduced Vision
A Golden Vision Clinic Extra
There are various things that can affect your vision. Most of them can be helped by a current prescription of glasses or contact lenses. The other factors that may decrease how well you see even with glasses may be helped by the following:
1. Increase the light. Have good general room illumination and read with a high intensity lamp or in a sunny window. Try not to have any glare but plenty of light.
2. Use a ruler to help you keep your place when reading.
3. A book holder or music stand can position your reading material at a good distance and hold it stable.
4. A variety of magnifying glasses are available at our office. They come with handles, stands to rest your book, and even with built‑in lights. Don’t be afraid of getting too close to your reading material.
5. Large print books and magazines are available. Contact your local library and they will either have or can get various large print materials. You can get The New York Times and the Readers Digest in large print.
6. Sit as close to the TV as you can to help you see. Use the largest screen TV as possible.
7. When sending or receiving letters try to use bright yellow paper with a black felt pen. You can also add a yellow filter over other materials to increase contrast. They are available here at our office.
8. Have your vision checked regularly to obtain the maximum from the most recent prescription.
Some lenses can be designed to help you read at a very close distance while other special designs can assist your seeing distance things.
There are also many techniques and resources that are available to help.
Macular Degeneration
 Age-Related Macular Degeneration (AMD) is the leading cause of severe vision loss in adults over age 50. It is a disease that affects both eyes with the average age of visual loss in the first eye being 65 years. Involvement of the second eye has an increase in incidence potential each year. The degeneration impairs the macula, which is the part of the retina used for central vision, thus, making driving, reading and close work difficult or impossible. Peripheral vision is spared. Partial vision aids which include hand magnifiers and high magnification spectacles are the only treatment/therapy available – we have these for you to examine. There is no “cure” for macular degeneration and it can get worse. Early detection from macular degeneration is the most important factor in determining if your eyes can be treated. This can be accomplished by covering one eye at a time and observing if straight lines, letters and numbers appear bent, multiple, blank spots or jumbled. You should check your vision in this way frequently for these specific changes that may mean you have macular degeneration. If you see any problems with your vision similar to these, make an appointment immediately.
Age-Related Macular Degeneration (AMD) is the leading cause of severe vision loss in adults over age 50. It is a disease that affects both eyes with the average age of visual loss in the first eye being 65 years. Involvement of the second eye has an increase in incidence potential each year. The degeneration impairs the macula, which is the part of the retina used for central vision, thus, making driving, reading and close work difficult or impossible. Peripheral vision is spared. Partial vision aids which include hand magnifiers and high magnification spectacles are the only treatment/therapy available – we have these for you to examine. There is no “cure” for macular degeneration and it can get worse. Early detection from macular degeneration is the most important factor in determining if your eyes can be treated. This can be accomplished by covering one eye at a time and observing if straight lines, letters and numbers appear bent, multiple, blank spots or jumbled. You should check your vision in this way frequently for these specific changes that may mean you have macular degeneration. If you see any problems with your vision similar to these, make an appointment immediately.
Recent studies have suggested specific formulas of vitamins and antioxidants that help prevent further deterioration of the macula. The AREDS (Age Related Eye Disease Studies) formulas are widely available. In addition, aerobic exercise which will increase blood flow, thus increasing oxygen supply to the macula is advised. Aerobic exercise includes walking, running, swimming, aerobics and biking. There is no known cause of this blinding disease but annual eye exams, vitamins, aerobic exercise, good sunglasses, and a diet as if you were a cardiovascular diseased patient may help in prevention. The sooner macular degeneration is diagnosed the sooner you can be helped with low vision aids, medications, and laser therapy.
There is growing evidence that ultra-violet radiation may break down the retina earlier in life.
While we live longer, this could leave your last years impacted. Do not wait until this dispute is
settled to protect your eyes….use the best sunglasses!!!
Migraines
 Migraines trouble many people, young and old. They are defined not by their severity, but by their classical pattern. Ocular migraines typically are initiated by what is called visual phenomena; that is, it occurs before the headache-some strange visual phenomena that lasts for about 20 minutes. During that time, your vision may be affected in one or both eyes. The center vision or part of the side vision may be blank; you also may have flashing, scintillating lights; or there may just be something distorted about your vision.
Migraines trouble many people, young and old. They are defined not by their severity, but by their classical pattern. Ocular migraines typically are initiated by what is called visual phenomena; that is, it occurs before the headache-some strange visual phenomena that lasts for about 20 minutes. During that time, your vision may be affected in one or both eyes. The center vision or part of the side vision may be blank; you also may have flashing, scintillating lights; or there may just be something distorted about your vision.
Following that you may or may not receive a headache, which can be mild, moderate, or severe; may last a short time or persist for several days. Typically, if you are able to vomit, that will terminate the headache.
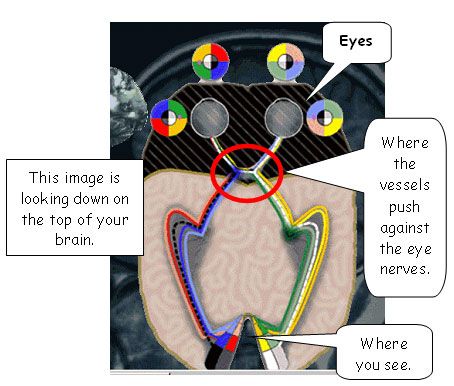
The theory of what causes the headaches is that swelling occurs in the blood vessels that flow into your brain. Since these vessels surround the optic nerve, the swelling pushes on the optic nerve and either shuts off its transmission or stimulates it to see flashes. As the swelling decreases, it eliminates the visual component but then may lead to a headache.
Our doctors suggest that if you are troubled by these repeatedly, it would be best to consult your physician to have them prescribe a medication to abort them.
Pingecula and Ptyergium
 A Pinguecula is a raised area that often appears whitish-yellow and is usually located on either side of the white part of the eye. This is not cancerous, or a cataract, but should be monitored. A Pterygium is very similar to a pinguecula except that it is located either totally or partially on the cornea (the clear window of the eye), and does offer far more threat to your sight.
A Pinguecula is a raised area that often appears whitish-yellow and is usually located on either side of the white part of the eye. This is not cancerous, or a cataract, but should be monitored. A Pterygium is very similar to a pinguecula except that it is located either totally or partially on the cornea (the clear window of the eye), and does offer far more threat to your sight.
What are the causes?
EXPOSURE TO SUN, WIND, DUST, POLLEN, and POLLUTION
Increased exposure causes irritation to the eye. Just like a callous on your hand, your body reacts by forming a thickened tissue area to protect itself from these irritants.
Is there any treatment?
PROTECTION FROM SUN & WIND, UV SUN PRESCRIPTION AND KEEP MOIST
Since we can not totally remove ourselves from the causative factors, we must minimize our exposure to these irritants to decrease the effects of them.
Since pinguecula and pterygium are most often caused by exposure to the sun’s ultraviolet rays, wind, dust or other irritants, our doctors suggest that it is best to limit exposure to all of these by wearing a good pair of sunglasses that provide complete protection for your eye against all potentially dangerous rays. A good rewetting drop helps to eliminate some of the irritation and helps to keep the eye moist to reduce friction of the lids while blinking (do not use Visine/Murine type of products). This can also be accomplished by adding a UV-400 coating to your regular prescription lenses. Goggles are highly recommended if you work in an area that is dusty or exposes you to chemical irritants.
Styes
 A stye is a clogged gland, on your eyelids, that is backed-up, swollen and inflamed. They can be tender to the touch. The procedure for care is:
A stye is a clogged gland, on your eyelids, that is backed-up, swollen and inflamed. They can be tender to the touch. The procedure for care is:
1. Clean your eyelids and lashes daily with a “Q-tip” or clean wash cloth and “no more tears” baby shampoo, followed by adequate rinsing.
2. A mild to hot compress should be used five times daily, for five minutes, for three weeks, on the affected eyelid. As long and as frequently as you can. While watching TV or another quiet activity you can microwave the hot compress usually about 10 seconds (be careful with the heat).
3. We may prescribe an eye ointment that you should rub into the lid and lashes of the affected area.
We recommend that you return for a re-check in our office in three weeks to determine progress. If the stye opens, secretion will drain from it. It is best to continue the care routine for at least one week after this occurs, to keep the gland opened and draining.
Subconjunctival Hemorrhage
A subconjuctival hemorrhage is a common disorder that usually occurs spontaneously in only one eye and may affect any age group. Its sudden onset and bright red appearance can be very alarming. The hemorrhage is caused by the rupture of a small blood vessel in the conjunctiva, which lies over the sclera (white part of your eye). It is very much like a bruise; but while your skin is translucent, allowing a bluish appearance, your conjuctiva is transparent, allowing the redness of the blood to show through. The subconjunctival hemorrhage appears as a flat, deep-red hemorrhage under the conjunctiva, and may be sufficiently severe to cause a traumatic “bag of blood” to protrude over the lid margin.
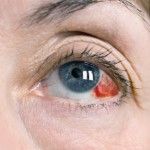 This hemorrhage is sometimes preceded by a bout of severe coughing or sneezing. It may be induced by a major or minor trauma to the eye; or it may just appear as a spontaneous hemorrhage. In rare instances hemorrhages occur in both eyes and are recurrent. In this case, the possibility of blood disease should be examined. Occasionally, bacterial or viral infections my be associated, accompanied by discomfort and discharge.
This hemorrhage is sometimes preceded by a bout of severe coughing or sneezing. It may be induced by a major or minor trauma to the eye; or it may just appear as a spontaneous hemorrhage. In rare instances hemorrhages occur in both eyes and are recurrent. In this case, the possibility of blood disease should be examined. Occasionally, bacterial or viral infections my be associated, accompanied by discomfort and discharge.
In the absence of infection or any trauma to the eye, treatment is unnecessary. The hemorrhage usually absorbs in two weeks with no therapy. Warm compresses generally will have it cleared up in 14 days. Blood thinners, including aspirin, may influence this situation. If it reoccurs, discuss this with your general practitioner.
If subconjunctival hemorrhage occurs and you have any questions, please feel free to get in touch with us.
If you have any other questions or concerns, please feel free to contact our office at any time for more information. 303-728-20/20
